
Memory Loss: Differentiating Dementia from Normal Aging
June 19, 2020 | Blog | Reading Time 8:00 Minutes

As individuals age, they often begin experiencing some difficulties with memory. But how can you tell the difference between normal aging, dementia and Alzheimer’s disease?
Dementia and memory loss are closely associated, but although similar symptoms can appear with various types of memory challenges, there are some significant distinctions.
Is Dementia a Normal Part of Aging?
No, dementia is not a normal part of aging. Dementia is a progressive disease that causes cognitive function to break down abnormally, causing cognitive and physical symptoms that worsen over time. Normal aging is much more minor, with changes resulting from a natural slowing or decrease in efficiency in the body.
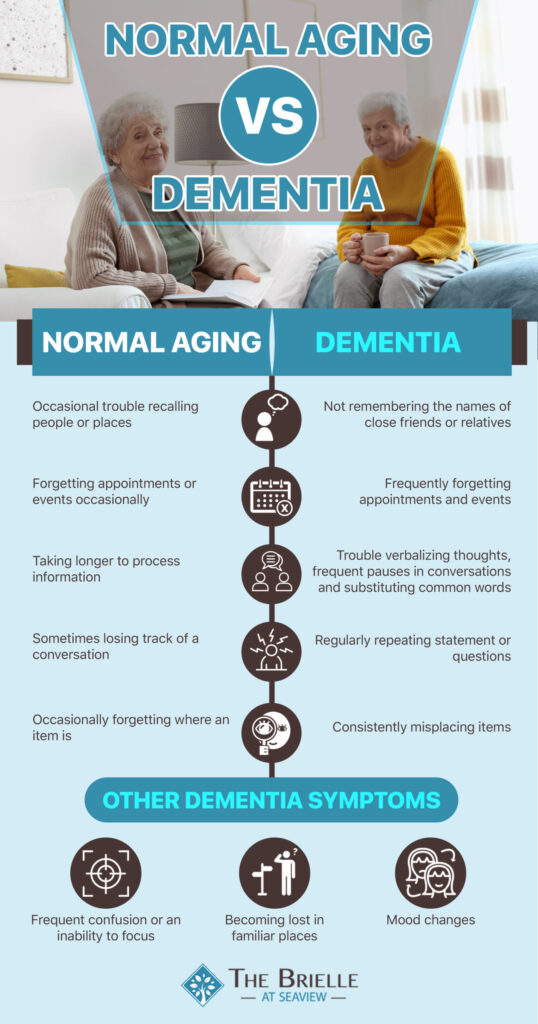
Normal Aging vs Dementia
In the normal aging process, the brain and body begin to slow, although a person’s intelligence level remains relatively steady. You or your relative may begin to experience some changes in memory that can manifest as trouble recalling names of places and people. You also may find that it takes longer to register certain information and that mental and physical flexibility decreases. Dementia, on the other hand, has more frequent and disruptive symptoms.
How can you tell if memory troubles indicate dementia and a need for memory care, rather than typical aging?
Dementia: A Set of Symptoms
Many people think that dementia constitutes a diagnosis in and of itself, but it describes a set of symptoms that can result from several different disorders of the brain.
The symptoms that dementia encompasses revolve around mental deterioration with a level of severity that affects the sufferer’s daily life. If you begin experiencing dementia, you may notice signs in a variety of different brain functions: recalling recent information, understanding symbols and maps, writing and speaking, reasoning, solving problems and other comprehension issues.
The Loss of Nerve Cells in Normal Aging and Dementia
Adults experience a loss of nerve cells in normal aging and dementia, but at different levels of severity.
The loss of nerve cells in normal aging is minor and is combined with nerve cells passing messages more slowly. This causes adults to take longer to process new information or recall old memories. The impairment is typically subtle and does not cause difficulty with daily tasks or independent living.
The loss of nerve cells in dementia is more severe, with the loss of nerve cells impacting the ability to think clearly and solve problems. How soon and how severe the loss of nerve cells is in dementia, as well as the symptoms it causes, varies based on the type of dementia an individual has.
Is Alzheimer’s Disease Different than Dementia?
Alzheimer’s disease is the most common of several types of dementia. Over time, the disease causes damage to the brain’s nerve cells with symptoms worsening as an increasing number of cells suffer damage. In Alzheimer’s disease, there is also a loss of nerve cells as part of the dementia that goes above and beyond the minor loss of nerve cells in normal aging.
The disease occasionally strikes people in their 40’s and 50’s or even younger, but sufferers tend to be over the age of 65. Alzheimer’s patients often initially notice symptoms like forgetfulness that can affect their work and home lives.
Additional symptoms include changes in mood along with misplacing items, repeating statements or questions, becoming confused or lost, and having problems with multitasking and verbalizing thoughts. There is no cure for Alzheimer’s, but treatments can help control the disease, especially when it is diagnosed early in its progression.
Additional Forms of Dementia
In addition to Alzheimer’s, other forms of memory loss include vascular dementia, also known as cerebrovascular disease — thought to be the second-leading cause of dementia. In vascular dementia, blood flow is blocked to portions of the brain, which kills some cells and can cause varying symptoms depending on the affected areas of the brain.
Vascular dementia symptoms can include problems with focus, confusion and memory loss and changes can occur gradually or suddenly. In some cases, a patient may experience rapid changes followed by a period of stabilization. Development of vascular dementia can be linked to chronic conditions like diabetes, heart disease, high cholesterol and high blood pressure.
Lewy body disease is a form of dementia in which proteins become deposited in brain nerve cells, causing symptoms such as impaired judgment, confusion and trouble with memory. Patients also can experience changes in movement abilities such as shaking, stiffness, trouble with balance and a shuffling form of walking. In addition, hallucinations, impaired facial expressions and significant sleepiness during the day can result.
In mixed dementia, patients can experience vascular dementia and Alzheimer’s disease at once. Research indicates that nearly half of individuals suffering from dementia may have symptoms of both forms of disease.
The rare frontotemporal lobar degeneration typically impacts the sides and front of the brain, and it often occurs in younger patients. The disease can advance more rapidly than Alzheimer’s, with patients initially showing alterations in judgment, social skills and overall personality. Individuals with the disease may seem to become coarse or even rude, and they may display poor behaviors relating to personal and financial issues.
Other forms of dementia include Creutzfeldt-Jakob disease (CJD) and Huntington’s disease. There are two types of Creutzfeldt-Jakob disease, one of which is caused by a genetic mutation. The second type usually occurs in adults between the ages of 45 and 75 and has no known cause but spurs a rapidly-progressing form of dementia that is fatal. Huntington’s disease is caused by a gene defect that affects 1 in every 10,000 people. Most adults start to experience Huntington’s disease in their 30s or 40s with symptoms including jerking movements, slower thought processes and trouble finding the right words.
Spotting Cognitive Decline: How to Tell if Someone Has Dementia
If a friend or family member is showing signs of memory trouble, how can you tell if the problem is a form of dementia or simply a normal effect of aging? In some cases, mild cognitive impairment (MCI) may serve as an intermediate step.
In MCI, an individual may have problems that do not hinder daily life but that are noticeable and register on mental functioning tests. Individuals suffering from MCI may be at increased risk for the development of Alzheimer’s disease, especially in cases that primarily center around memory. Not all MCI patients develop Alzheimer’s or another form of dementia, however.
Understanding the risk factors for MCI can help you determine if your loved one may need medical evaluation. They include:
- Chronic conditions such as diabetes, heart disease and high blood pressure.
- Dementia cases that run in the family.
- Suboptimal nutrition.
- Stress, depression and other psychological issues.
When a loved one’s condition progresses to dementia, it should become apparent that a problem exists beyond normal aging. Dementia typically includes several types of cognitive impairments, in language, working memory, verbal abilities, executive function or spatial memory.
In most cases, a patient must demonstrate an impaired ability to live independently — including activities like handling finances, taking care of a household, cooking, bathing and dressing — for a medical professional to diagnose a form of dementia. Because specific symptoms can vary, it’s important to discuss any changes you notice with your family member’s doctor.
Caring for a Friend or Relative with Dementia
Following a diagnosis, dementia often progresses through three distinct phases: mild, moderate and severe. As the disease moves into the moderate phase, your loved one may require more assistance with activities of daily living, including personal hygiene. At the moderate phase, you also may begin to feel challenged with providing care.
In addition, if your relative lives with you, your home may require some changes like removal of tripping hazards, installation of brighter lighting and the addition of safety latches on doors.
As dementia progresses to the severe stage, your loved one may experience very limited mobility and problems with eating, drinking and toileting that require constant care. If you are providing care for your loved one, it’s critical to take steps to control your own anxiety and to get support.
Don’t be afraid to ask other family members and friends for help, and consider using resources like your local chapter of the Alzheimer’s Association.
Compassionate Memory Care in Staten Island
At The Brielle, our highly trained staff members provide exceptional Staten Island memory care in our Valeo Neighborhood. Our team has extensive experience working with individuals with multiple forms of dementia, including providing Alzheimer’s care. For those who are experiencing normal aging, we offer assisted living, which provides help with daily tasks and a staff that can help residents understand if their symptoms are normal aging vs dementia.
All our residents benefit from a holistic wellness program that helps them continue living a vibrant life in a respectful atmosphere. To find out more about our memory care program, please contact us.
